

We ease the transition into risk contracts and value-based reimbursement.
Poor alignment of provider performance with clinical and financial objectives, antiquated reporting systems, and inefficient provider engagement programs are preventing health plans from consistently achieving important goals including:
4 and 5 STAR CMS Ratings
Increased HEDIS/Quality Outcomes
Improved MLR
As a result, Health Plans are losing between 15-25% of their potential revenue. The missing link between low and high performing health plans is a robust provider engagement initiative that tracks performance and incentivizes the desired behaviors. iMLR is the tool that makes that possible.
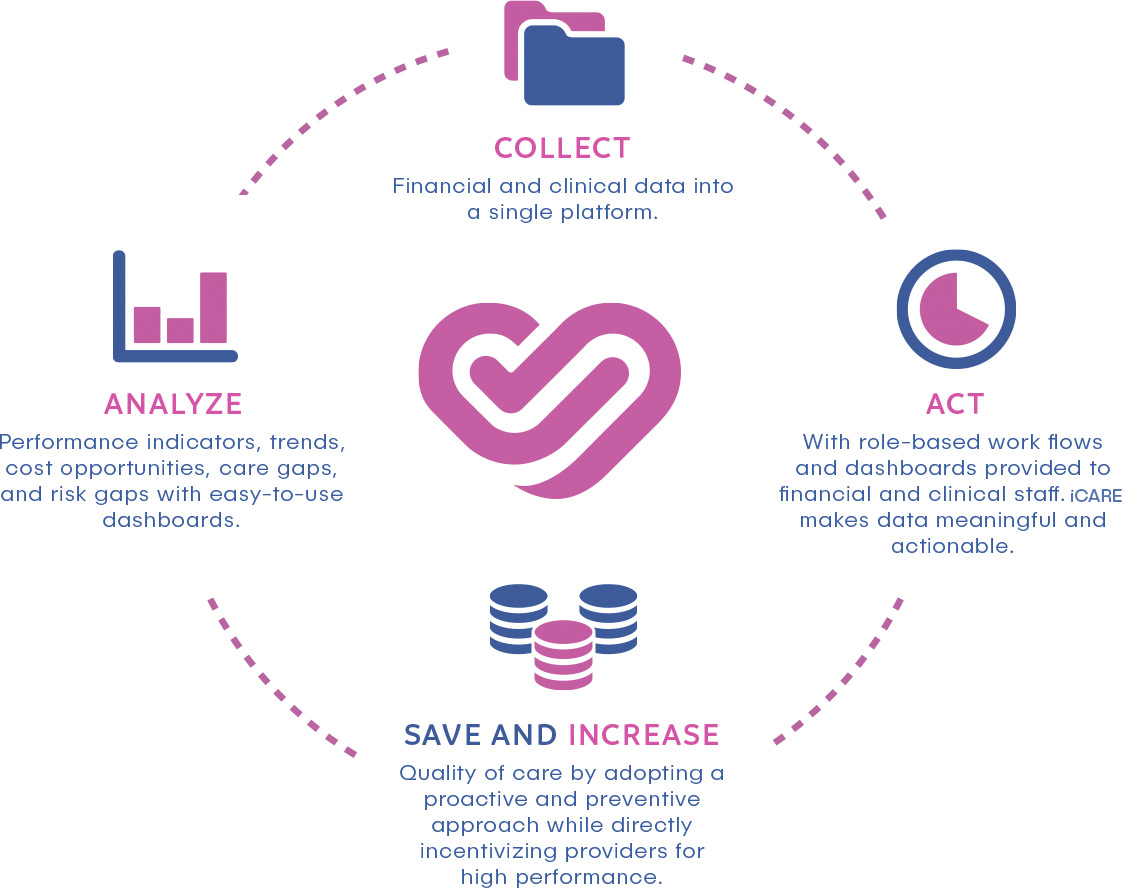
We bring Solutions to Healthcare Organizations through Data Analytics

Performance indicators, trends, cost opportunities, care gaps, and risk gaps with easy-to-use dashboards.
Financial and clinical data into a single platform.

With role-based work flows and dashboards provided to financial and clinical staff. iMLR makes data meaningful and actionable.

Quality of care by adopting a proactive and preventive approach while directly incentivizing providers for high performance.
In a typical system, physician performance cannot be easily measured on a timely basis. As a result, good providers are not incentivized to improve performance measures and poorly performing providers are not identified and given proper support.

It would be our pleasure to answer questions about our solution or to demostrate how iCare how our technology delivers value to our clients. Click below to schedule a call.


